CRUCIATE LIGAMENT SURGERY — INDICATIONS, METHODS, AND SUCCESS RATES
A crack or pop in the knee, severe or minor pain, and swelling in the joint: A cruciate ligament tear is a very common injury and must be treated in all cases — whether conservatively using physiotherapy, or surgically.
In this article, Dr. Gäbler explains the methods available for cruciate ligament surgery and the advantages and disadvantages associated with each technique.
Table of Contents
- When does a cruciate ligament tear require surgery?
- Cruciate ligament surgery: What are the methods?
- Cruciate ligament surgery: When can I play sports again?
- Success rates and conclusion
More questions?
Our experts are happy to help you
Just give us a call!
When does a cruciate ligament tear require surgery?
Several factors decide whether surgery is required after a cruciate ligament tear:
- Degree of instability
- Age of the patient
- Activity level
- Existing accompanying injuries
The higher your level of physical activity, the more likely it is that an operation will be recommended. If your physician recommends cruciate ligament surgery, the next step is a detailed discussion about which surgical method is best for you.
Cruciate ligament surgery: What are the methods?
Depending on the severity of the injury and level of athleticism, different surgical methods can be used to treat a cruciate ligament tear. Your specific case must be evaluated in a detailed discussion with your doctor.
STG method: Tendons from the back of the knee
The name STG method is an abbreviation of the names of the tendons used for the graft (semitendinosus and gracilis tendons). Both are knee flexor tendons that can be removed without the knee joint experiencing any significant loss in strength or function.
The advantage dieser Technik besteht im kleineren Hautschnitt und darin, dass die Patient*innen mit der STG-Technik meist weniger über postoperative Schmerzen klagen als jene mit einem Transplantat von Quadrizeps- oder Patellasehne. Vor allem treten die typischen Schmerzen an der Entnahmestelle der Knochenblöcke nicht auf. Weiters gibt es die Probleme wie Kniescheibenbruch and Patellasehnenriss nicht. Und auch nicht die typischen Muskelprobleme nach Entnahme der Quadrizepssehne.
Ein deutlicher Nachteil der Technik besteht darin, dass vor allem die Beugekraft im Kniegelenk um ca 10%, aber auch die Innenrotation des Unterschenkels eventuell etwas geschwächt (dies fällt vor allem Hochleistungssportler*innen auf). Ein weiterer Nachteil liegt darin, dass in 10 – 20 % der Fälle (nach manchen Literaturangaben auch in einer höheren Anzahl) ein Nerv geschädigt wird – dies führt zu einem (meist vorübergehenden) Taubheitsgefühl an der Unterschenkel-Innenseite (in sehr, sehr seltenen Fällen auch zu brennenden Nervenschmerzen). Und es sollte diese Technik nicht bei PatientInnen mit Valgusfehlstellung (= X-Bein) angewendet werden, da die Hamstrings der Fehlstellung im X-Bein entgegenwirken.
STG method: Procedure
The operation begins with an arthroscopy (i.e., an examination of the knee joint) and the removal of the remains of the torn cruciate ligament. Any damage to the meniscus or cartilage can also be treated at this point. If the cruciate ligament insertion point is still sound, it can be left in place, thus preserving the body’s own receptors. This is followed by a freshening of the bone at the cruciate ligament insertion sites.
In contrast to the BTB graft, the incision made below the kneecap is only about 3 cm long, allowing the two knee flexors to be removed and a socket to be drilled into the bone tunnel in the lower leg.
The socket for receiving the transplant is then drilled into the thigh, the STG graft is inserted, and a special technique anchors it into position. This method generally uses bioabsorbable screws that slowly dissolve after a few years and are reabsorbed by the body.
Even self-dissolving screws, however, can also cause problems (including hypersensitivity to foreign bodies and bone cavity formation), which is why Dr. Gäbler and his team prefer the “all-inside” technique without screws.
All-inside reconstruction: Lower risk and less pain
To ensure that the operation is as gentle as possible, incurs less pain, and has a lower surgical risk, Dr. Gäbler uses the all-inside technique for cruciate ligament reconstruction: A single tendon (gracilis or semitendinosus) is quadruplicated and inserted into a bone tunnel using small incisions.
This method is far gentler than the continuous bone tunnels of earlier methods, which caused massive trauma to the bones and skin of the legs and were associated with significantly greater pain and postoperative complications. The smaller incisions significantly reduce tissue damage and significantly improve cosmetic results.
Dr. Gäbler himself is often astounded by how much improvement injured athletes experience after an all-inside operation, especially when compared to conventional methods.
With the all-inside technique, anchoring is achieved using endobuttons, also the method of choice when treating torn cruciate ligaments in children. Immobilization of the knee is only necessary if other injuries are present.
BTB (Bone-Tendon-Bone): Kneecap or patellar tendon
BTB, short for bone-tendon-bone, refers to the grafting of a rectangular bone fragment, a section of tendon, and then another bone fragment.
This technique uses the kneecap or patellar tendon, the tendon that connects the kneecap with the lower leg and thus plays an important role in stretching.
The great tensile force of the tendons used is an advantage of this technique, as is the fact that the bone fragments heal quickly, allowing the patient to rapidly achieve optimal stability of the knee joint and therefore begin athletic training again relatively soon.
The disadvantage of the technique is that about 10% of patients complain of pain at the points where the bone fragments were harvested (anterior knee pain) that is especially noticeable when kneeling. Complications such as kneecap fractures and torn tendons are also known to arise. The primary problem with the method, however, is that long-term studies seem to indicate that almost all patients with a BTB transplant display some degree of pronounced retropatellar osteoarthritis (cartilage damage behind the kneecap) after 20 years.
BTB technique: Procedure
The operation begins with an arthroscopy (i.e., an examination of the knee joint) and the removal of the remains of the torn cruciate ligament. Any damage to the meniscus or cartilage can also be treated at this point.
This is followed by a freshening of the bone at the cruciate ligament insertion sites. Many surgeons now make a large incision above the tendon, through which the entire surgical area can be observed and the tendon can be recovered. As this method often leads to nerve injuries and numbness, Dr. Gäbler prefers to make two smaller incisions above the bone fragments and to salvage the middle part of the tendon and bone section (a rectangular bone fragment of approximately 1.5 cm long and 8 mm wide taken from the tip of the kneecap and the tibia head) using a minimally invasive keyhole technique.
The tunnels for receiving the bone blocks are drilled near the former insertion point and base of the anterior cruciate ligament, and the cruciate ligament preparation is inserted and anchored into position using special titanium interference screws. Immobilization of the knee is only necessary if other injuries are present.
Cruciate ligament suture (reinsertion and refixation)
If the ACL is torn at the top of its anchor point (in about 10-20% of cases, seen more often in children and adolescents), it is possible to reaffix it using special dowel bolts. This method has the advantage of being much gentler than other methods. The ACL and all its receptors are preserved, and no tendons must be removed.
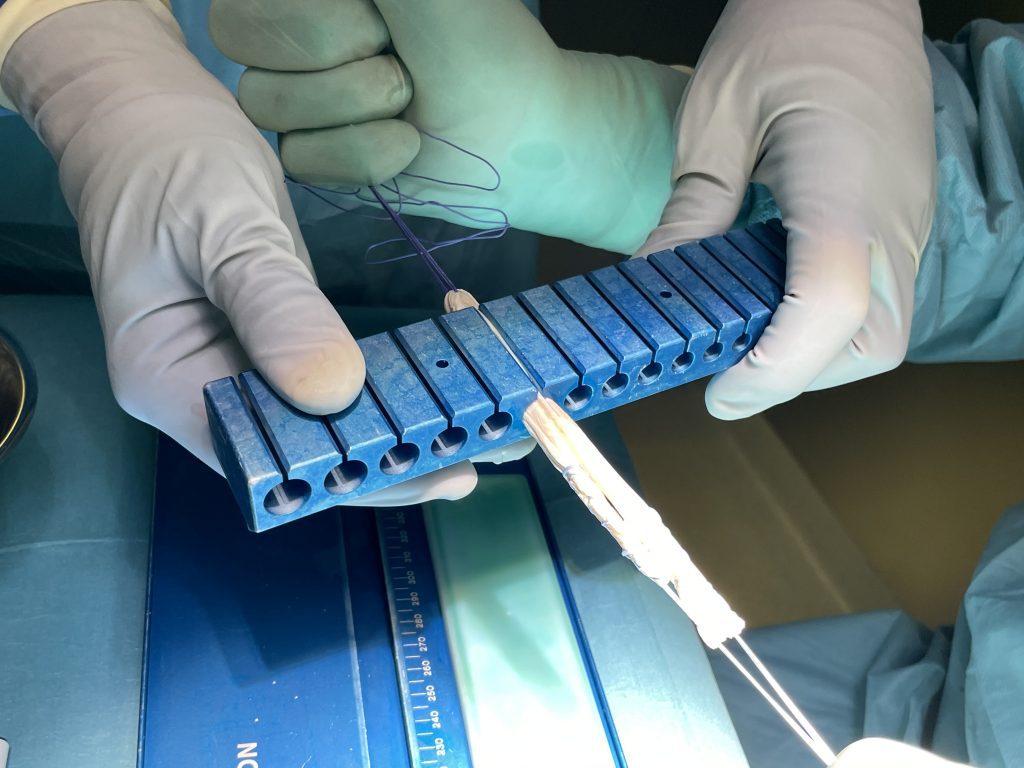
An ACL reinsertion can be elegant and minimally invasive, requiring only three very small incisions 4-5 mm in length. During the procedure, the ACL is looped with a special retention stitch and then reaffixed with a dowel pin at the correct point (see Fig. 1).
In order for healing to progress optimally, Dr. Gabler makes tiny incisions in front of, above, and behind the cruciate ligament (see Fig. 2). These incisions allow stem cells to emerge from the bone, which stimulate a natural healing response that supports ACL recovery right where it is needed.
Dr. Gäbler has used this technique on several hundred patients with excellent results. The re-rupture rate (i.e., the likelihood that treatment fails) is less than 0.5% if the diagnosis was correct.
Quadriceps tendon
This tendon, located above the kneecap, is used in revisional operations when the STG and BTB have already been removed or are not available for other reasons.
Allograft (Donor Tendon Graft)
In contrast to an autograft (the patient's own tendon), an allograft is a donor tendon. An allograft is often one of the last options for achieving sufficient knee stability when patients have already torn their anterior cruciate ligament (ACL) several times. After the third cruciate ligament tear at the latest, there is a lack of suitable endogenous tendons for a new cruciate ligament reconstruction. Then donor tendons are the perfect alternative. With an allograft, the operation time is also significantly shorter, the pain after the operation is significantly less - and the rehabilitation is faster, because no own tendon had to be removed - thus all possible complications that can occur with the removal of an endogenous tendon are also eliminated.
In fact, allografts are often the first choice for top athletes because they do not want to remove tendons - especially in elite sports, a few percent more or less muscle performance can make the difference between winning and losing - and if a tendon has been weakened or is missing altogether, the road back to former top performance is often long and arduous. One example of an allograft recipient is Italian ski racer Sofia Goggia, who has gone from victory to victory this season with a donor tendon in her knee joint (she herself succinctly says she is winning with a dead man's cruciate ligament).
In very young athletes (who do not earn their money with high-performance sports), we recommend using autologous tendons for the primary reconstruction of the ACL. In this patient group, higher rupture rates have been demonstrated with the primary use of allografts - however, the reason could be that the return to sports is often too early due to the lower pain and significantly faster rehabilitation.
In the USA, the use of allografts for ACL reconstruction has been established for decades. In Europe, this technique has only been increasingly used for a few years. However, the use of allografts has clear advantages: they can be ordered as needed. Diameter and length can be customized. Numerous studies show that concerns about implant rejection, excessive immune response or transmission of infections are unfounded.
The question naturally arises with donor transplants: are these transplants safe and how is possible transmission of infection prevented?
Here we can reassure, because the legally mandated measures to ensure the safety of biomaterials such as allografts apply to all infectious diseases, from HIV to COVID.
Safety measures for the allografts we use include donor history, serological testing using antibody screening and PCR (polymerase chain reaction), continuous microbiological testing). Only 4% of all donors are accepted after the screening process. This is followed by the complex wet-chemical disinfection and removal of blood, bone marrow and protein (= BioCleanse® Tissue Sterilization Process). This process is done without irradiation, unlike other allografts (therefore the re-rupture rate of the donor grafts we use is extremely low).Since 1995, there has not been a single transmission of infection in more than 4 million bio-implants treated with this method.
Cruciate ligament surgery: When can I play sports again?
When and to what extent you can return to an exercise regime after cruciate ligament surgery should always be clarified with your doctor. In any case, you should follow your doctor’s instructions precisely, as returning to training too soon can cause additional knee injuries.
Success rates and conclusion
The goal of a cruciate ligament operation is to maintain stability in the knee through the best possible reconstruction. In most cases, this is successful. Cruciate ligament surgery is always a technically demanding operation that should only be performed by an experienced surgeon.
Under the guidance of highly experienced knee surgeon Dr. Christian Gäbler, the knee specialists at the SPORTambulatorium Wien – Center for Orthopedics and Sports Traumatology provide expert and personalized care of your knee ligament injuries using the most up-to-date arthroscopic surgical methods, as well as non-surgical treatment whenever possible.
Make an appointment online using the contact form or by phone: 01 4021000
More questions?
Our experts are happy to help you
Just give us a call!