The Meniscus
The meniscus is made up of fibrous cartilage (similar to a spinal disc) and absorbs shock as well as stabilizing the knee joint. It is possible to damage the meniscus through acute injury and/or degenerative wear.
Acute injuries generally occur while doing sports, but can also happen by a movement as simple as standing up, if the meniscus is pinched and torn by a rotational movement at the same time.

Bei diagnostiziertem Meniskusschaden ist eine Operation oft erforderlich, das muss aber genau beurteilt werden, denn nicht jeder kaputte Meniskus muss auch operiert werden. Meist führt ein Meniskusriss sehr rasch zu Knorpelschäden, daher ist eine sorgfältige Evaluierung der Vor- und Nachteile einer Operation ausgesprochen wichtig.
Eine MRI Abklärung ist immer angeraten, da es auch Meniskusschäden gibt, die nicht operiert werden müssen.
Prolonged athletic restrictions are not necessary after a meniscus operation. It should be kept in mind, however, that there is a correlation between the degree of resected meniscal tissue and the statistical probability of early onset osteoarthritis.
A return to sports depends on the surgical method and the extent of damaged tissue.
More questions?
Our experts are happy to help you
Just give us a call!
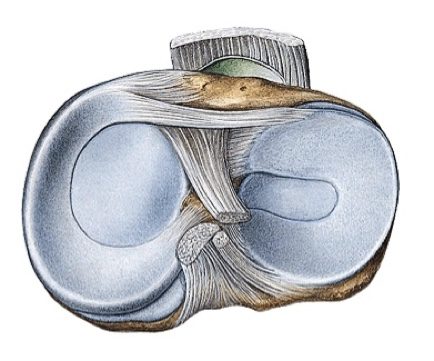
The medial and lateral menisci play a shock absorbing role in the knee. They are crescent or sickle-shaped structures located between the thigh and lower leg. The meniscus (similar to the intervertebral discs in the spine) consists of fibrous cartilage, a rubber-like substance, and, in addition to its shock absorbing function, also guides movements of the knee joint and stabilizes the joint together with the ligaments.

Even with menisci, acute injuries (often sporting injuries sustained during skiing, football, etc., however a meniscus injury can also be caused by a significant rotation when standing up from a crouch), can be differentiated from degenerative, i.e. "wear-related" damage . Injuries of the medial meniscus are significantly more common than injuries of the lateral meniscus, as the medial meniscus grows firmly together with the Collateral Ligaments .

In the event that meniscus damage is diagnosed, it is preferred to have an operation (arthroscopy of the knee) very early on, even if there is no or very little pain, because a damaged meniscus causes ongoing wear on the cartilage, very quickly resulting in cartilage damage.
The irritation also rarely stops on its own as the meniscus is only very little blood in it and can rarely heal itself.
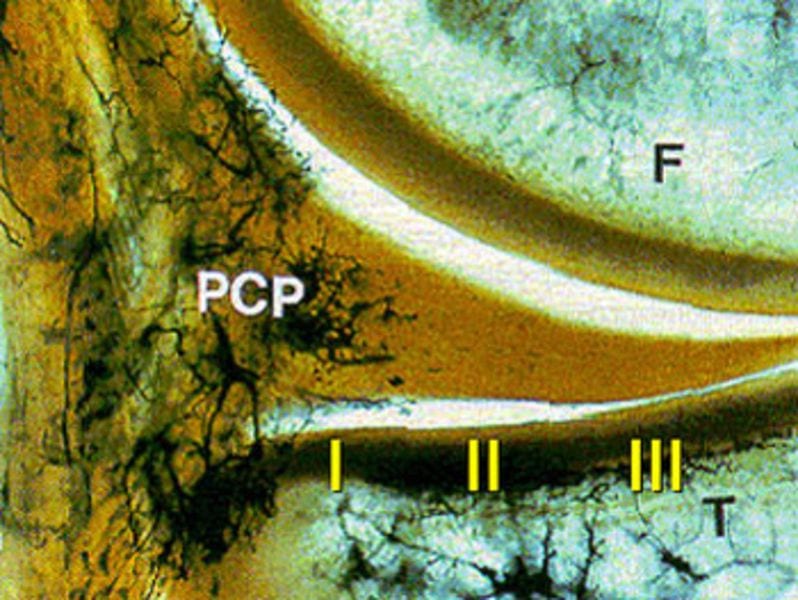
Strong healing generally only occurs in the red zone (Image 4). Perfusion and therefore healing capacity decrease medially until Zone III.
The constant wearing motion on the damaged meniscus in untreated meniscus injuries leads to recurring pain on exertion, impingement symptoms, swelling of the knee joint, and secondary damage to the cartilage surfaces and thus early-onset arthrosis.
Cysts occasionally form on the base of the meniscus, called a ganglion (or meniscus ganglion). A ganglion is usually filled with a jelly-like fluid. In the majority of cases, a meniscus tear is also present, and must be treated immediately. Removal of the ganglion alone, without rectifying the cause, usually has no great value.
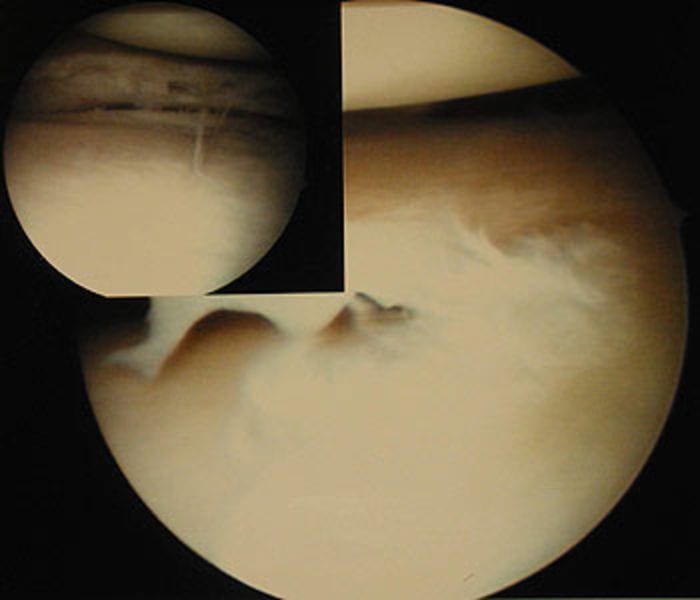
During arthroscopy of the knee joint , the damaged section of the meniscus is removed and the meniscus is carefully smoothed.
In order to minimize the risk of arthrosis that arises after a partial removal of the meniscus, it is possible to try to retain the meniscus. Suturing of the meniscus is only carried out in rare cases, primarily in Zone I (see Image 4).
The advantage of meniscus refixation is that it minimises the increased risk of arthrosis that exists after a partial removal of the meniscus.. The disadvantage of meniscus refixation is that patients may not put weight on the operated leg for up to six weeks - and even then, the rest of a repeat tear is relatively high. Healing conditions are only ideal if the meniscus refixation was done in Zone I (see Image 4).


FOLLOW-UP CARE:
After a meniscus operation (partial removal of the damaged meniscus), is it possible to immediately put weight on the leg, provided that pain levels permit it. Crutches are often only needed for a few days. Cycling or rowing machine training is possible after two weeks, running after four weeks, and ball sports and skiing after six weeks. After meniscus suturing and meniscus refixation, it is necessary to walk with crutches for four weeks with no weight on the leg, followed by two weeks with weight bearing permitted up to half the patient's body weight. It is often not necessary to immobilize using a splint, unless there are existing concomitant injuries, e.g. of the collateral ligament. Cycling or rowing machine training is possible after six weeks, running after twelve weeks, and ball sports and skiing after six weeks.
After a meniscus operation, no athletic restrictions are to be expected. Returning to the various types of sport depends on the operation method and the extent of the damaged meniscus tissue. It must be made clear, however, that there is a direct correlation between the extent of the resected meniscus tissue and the statistical likelihood of early-onset arthrosis. The more meniscus tissue that must be removed, the more likely it is that the patient will suffer from early-onset joint wear (arthrosis).
More questions?
Our experts are happy to help you
Just give us a call!