Achilles Tendon
The Achilles tendon is often overexerted while running and the resulting inflammation (achillodynia) is common. Unfortunately, if it becomes chronic, the condition can be protracted.
Typical symptoms are pain, swelling, and an overheated Achilles tendon. Runners typically first feel an uncomfortable pulling sensation in the tendon area. Sensitivity to pressure increases and swelling occurs. The pain is particularly severe in the morning and during the first few minutes of running.
When chronic, the tendon thickens and causes permanent pain.
Inflammation of the Achilles tendon can be the result of overexertion and training errors such as inadequate stretching and warming up, but can also be caused by leg axis problems and poorly fitted running shoes. More often than not, a combination of these factors comes together to create the underlying issue.
Along with regular physiotherapy, the triggering factors must, of course, be resolved, for example, by adjusting running shoes using treadmill analysis.
While the condition is acute, it is advisable to switch to other endurance sports. Cryotherapy, poultice wraps, and sports ointments are also recommended.
If the inflammation is already chronic, treatment consists of daily strengthening exercises, orthotic insoles, and physical therapy — all in combination with shockwave or Repuls red light therapy.
Particularly persistant cases can be treated with autologous blood (PRP) or cortisone, and in extreme cases surgery is also an option.
More questions?
Our experts are happy to help you
Just give us a call!
The Achilles Tendon, the strongest tendon in the human body, was considered to be the weak point of the otherwise invincible Achilles (Achilles heel) in Greek mythology. Ambitious runners will also have a story to tell about this tendon.

The function of the Achilles tendon is to bend the ankle, pulling the forefoot downwards with strength. This movement is crucial for pushing off the foot when walking and running.
The Achilles tendon is often overexerted while running and the resulting inflammation (achillodynia) is, unfortunately, common - and often also prolonged. Either the Achilles tendon directly at the area of attachment to the calcaneus or the tendon and the surrounding paratenon several centimeters above the attachment are affected. In the case of chronic achillodynia, a spindle-like thickening of the Achilles tendon occurs, together with persistent pain that varies in intensity.
Häufige Probleme der Achillessehne:
TREATMENT TIPS IN THE ACUTE PHASE
- Stop training (if possible, switch to another type of endurance training such as cycling, swimming, or aqua jogging until symptoms have subsided).
- Ice packs can help in the acute pain stage if you have nothing else at home. However, do not apply ice for more than ten minutes and never place it on bare skin.
- Cold curd compresses can help alleviate inflammation
- Sports plaster: Dr. Gäbler thinks highly of the Flector EP Plaster, which releases the anti-inflammatory active ingredient (Diclofenac) consistently over 12-14 hours, therefore often leading to a rapid improvement in symptoms. (This should obviously not be used in the case of Diclofenac intolerance, as it can cause skin irritations. Fortunately, this is extremely rare.)
- Sports ointments can also help. However, they have the disadvantage that the majority of the active substance is not absorbed by the skin but instead by the patient's socks.
- REPULS infrared therapy is a new, particularly gentle and fast-acting method of significantly accelerating the healing of inflammation. For more information, see Repuls Infrared Therapy
- A padded heel insert can be useful in the initial stage, but only short term as can become counterproductive!
Once free of pain, athletic training can start again. Heat therapy immediately prior to training is recommended in the initial weeks (e.g. with essential oil thermal ointments) in combination with consistent and thorough warm-up exercises. Stretching after training should be carried out consistently (this is true despite several unfortunate articles recently published claiming that stretching exercises are useless), preferably as a dynamic stretching program and with rotational exercises for the Achilles tendon. Moreover, after each training session, the sore tendon should be cooled with ice packs or cold curd compresses.
If in the chronic stage, treatment is quite different:
At this point, the best results are achieved by‚ using a combination of daily eccentric muscle exercises, orthopaedic inserts (to be primarily worn in day-to-day life) and physiotherapy in combination with Repuls infrared light treatments (see above).
Eccentric muscle exercises: A Swedish study showed that patients with chronic Achilles tendon symptoms were able to achieve a full recovery within 12 weeks if they carried out eccentric exercises consistently. It was astounding that all the athletes studied had already had treatment-resistant symptoms for two years.
The exercise involves standing on a step with the ball of the foot and lifting the heel slowly upwards (one can also do it with both foot for stability) and then slowly lowering the heel and pressing it down as far as possible, significantly stretching the Achilles tendon. The authors of the study also recommended wearing a heavy rucksack to add more weight to the stretch. Dr. Gäbler, however, feels that this is somewhat excessive, as the stretching is the important part, not the lifting the heel.
Such muscle exercises cause small vessels to necrotise on the one hand (and therefore also the painful nerve endings), and on the other, the exercises increase the production of Type 1 collagen, which heals and strengthens the tendon.
It often takes months, however, until symptoms actually improve, which is obviously very detrimental to any keen runner, as only very limited running is permitted during this time.
See also - Video
Accompanying therapy for athletes:
- Ice pack for a maximum of 10 minutes prior to and after training
- Eccentric stretching immediately after training
- Reduced running training up to a pain intensity of VAS 5 (on a scale of 0-10)
- Nitrolingual spray 2 x 2 puffs locally on the Achilles tendon for 6 months as an off-label use
- Balance training as part of a physiotherapy program
In case of persistent symptoms, the following treatments can also be carried out:
- Mesotherapy (3-5 sessions)
- Shock wave therapy (3-5 sessions)
Cortisone
Injections with cortisone are only indicated in truly treatment-resistant cases, although improvement with cortisone is often immediate and lasting.
Cortisone is an excellent inhibitor of inflammation (and can therefore be used to treat specific symptoms) and necrotiser of small vessels and therefore also painful nerve endings, which means rapid relief from pain.
Cortisone can, however, also cause deterioration in the blood circulation of the tendon if injected too close or directly into the tendon itself, therefore causing microscopically small sections of tendon to necrotise, which significantly increases the likelihood of a later Achilles tendon tear. The common yet incorrect injection of cortisone directly into the Achilles tendon has, due to its high complication rate, has led some doctors to completely refuse to administer cortisone (likewise not a helpful approach: the administration of cortisone (as with any other medication) must be considered carefully as an option.) Infiltration with cortisone should therefore not be carried out more than twice (within a short period of time) as it is probably more sensible to carry out a small, minimally invasive operation to remove inflamed sections of tissue.
PLATELET-RICH PLASMA INFILATRATION (ACP)
ACP (autologous conditioned plasma) is made from specially centrifuged blood removed from a vein in the patient's arm. This activates the thrombocytes (blood platelets), releasing proliferative substances (such as Platelet Derived Growth Factor, PDGF) and morphogenic proteins (Transforming Growth Factor, TGF) that are important for muscle, tendon, cartilage, and bone healing. New research shows that treatment with ACP can significantly accelerate and improve the healing of muscle injuries, as well as tendon and cartilage problems.
Further information about ACP infiltration available here.
Video about platelet-rich plasma therapy (ACP)
Surgical Methods:
CHRONIC ACHILLODYNIA

In the event of chronic symptoms, an operation may be indicated if conservative treatments fail.
The Endoscopic Achilles tendon decompression is a minimally-invasive operation method that often leads to excellent outcomes in cases of chronic achillodynia and Haglund’s deformity . The operation removes layers that have been altered by inflammation and mills off any ossification. Immobilization in a cast is required is required for 2–4 weeks after the procedure.
In very severe cases, a larger incision is necessary. The Achilles tendon is split lengthways and the central necrotic sections of the tendon are removed. The tendon can then be resutured.

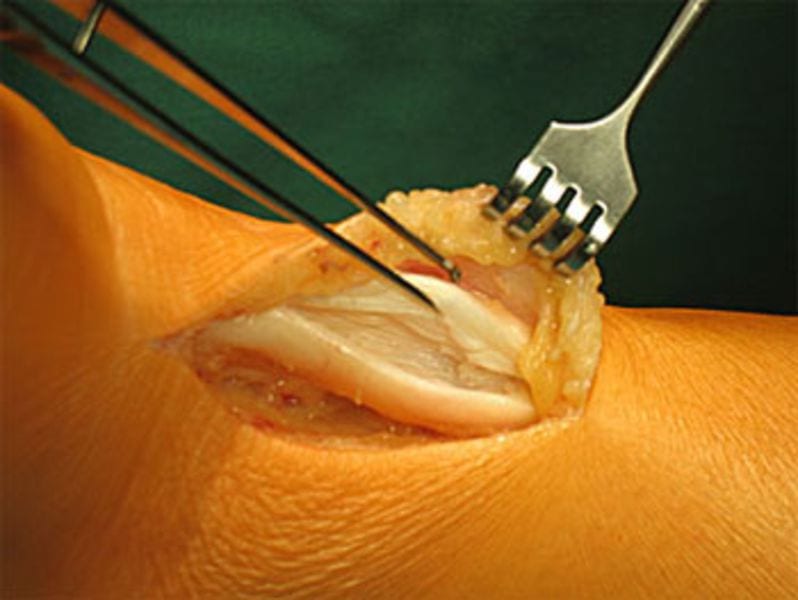
It is particularly easy to remove Haglund’s deformities using this method. The disadvantage is, of course, the somewhat larger skin incision.
Additional treatment options:
Extracorporeal shock wave therapy for achillodynia:
Extracorporeal shock wave therapy is a newer method of pain relief. It is suspected that pain is not alleviated by fragmentation but by the shock waves activating the self-healing processes of the cell. Shock wave therapy improves cell metabolism and deactivates pain fibers. Following multiple treatments, 60-80% of patients experienced alleviation of pain or even complete relief of symptoms. For Dr. Gäbler, this success rate is too low (in comparison with the excellent results of eccentric muscle exercises, consistent physiotherapy, and orthopaedic inserts), however it is a non-surgical method that can be undertaken in treatment-resistant cases.
Autologous Conditioned Plasma:
Treatment with autologous conditioned plasma (ACP) is a new type of treatment for chronic achillodynia and insertion tendinopathy. It has been known for a long time that the growth factors contained in human blood can positively affect a variety of different healing processes. ACP therapy works on the basis of this knowledge. Healing and the reconstruction of tendon tissue damaged or altered as a result of inflammation can be stimulated using concentrated growth factors.
How does ACP therapy work?
A small amount of blood is drawn from an arm vein for a blood test. A special process then separates the portion of blood containing the autologous regenerative and arthrosis-inhibiting components. The autologous solution obtained in this manner is injected into the affected tissue using a specially developed double syringe (Arthrex Double Syringe). This newly developed double chamber system ensures that the growth factors are obtained and injected in a sterile process that offers the highest possible level of safety. Note: There is still no scientific proof that this treatment helps or to what percentage healing success can be achieved, however patients suffering from arthritis are familiar with the positive effects and there are positive reports regarding use of this treatment.
ACHILLES TENDON TEAR
A sudden movement (such as starting to sprint or jumping when playing tennis), patients can suffer an Achilles tendon tear when the tendon suddenly contracts. Runners with chronic pre-damaged tendons are frequently affected, and incomplete tears of the Achilles tendon can also occur.
Another typical injury mechanism is a direct kick to the tendon, which can be incurred, for example, during a football match by a rough opponent. A clear “crack” is often heard when this happens.
Typical symptoms include pain and restriction of movement, and a definite indentation can often be felt in the Achilles tendon. The injured person is no longer able to stand on tip toes. A typical diagnostic indication is a positive Thompson test: Compression of the calf while the patient is kneeling does not lead to plantar flexion (flexion of the foot or the toes towards the sole of the foot), when compared to the uninjured side. If a diagnosis cannot be made with absolute certainty, an ultrasound or magnetic resonance imaging (MRI) should be carried out.
Treatment involves an operation to directly suture both tendon stumps, possibly strengthened using an autologous tendon (plantaris tendon). Conservative treatment is only useful if it is possible to verify by X-ray that both tendon stumps are well apposed in plantar flexion.
Several weeks of wearing a cast is then required. A “walker”, a boot-like support that protects the operated area, is more comfortable for the patient than a plaster dressing.
More questions?
Our experts are happy to help you
Just give us a call!